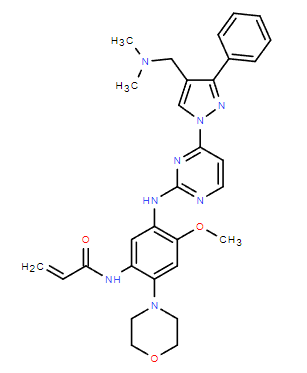
Chemical Name: Lazertinib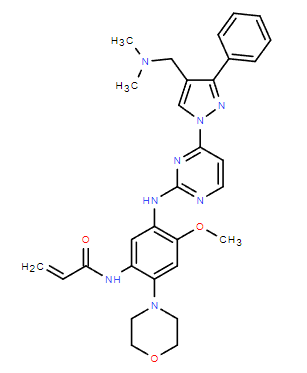
CAS No.: 1903008-80-9
Company: Janssen/Yuhan Corporation
Indication: non-small cell lung cancer
In July 2015, Genosco partnered with Yuhan Corporation to develop as well as commercialize Lazertinib.
In November 2018, Yuhan and Janssen signed a collaboration agreement whereby Janssen is responsible for the development, manufacturing and commercialization of Lazertinib in the unexpected region of South Korea.
On November 28, 2019, Janssen submitted a product-specific exemption application for Lazertinib to the European Medicines Agency, which was approved. As of March 2024, the drug has not been approved for marketing.
On January 18, 2021, the Korea Food and Drug Administration approved Lazertinib for the treatment of patients with EGFR T790M mutation-positive locally advanced or metastatic non-small cell lung cancer who have received prior EGFR-TKI therapy.
On December 23, 2023, Janssen submitted a supplemental Biologics License Application and New Drug Application to the FDA seeking approval of RYBREVANT® (amivantamab-vmjw) + Lazertinib for the treatment of patients with EGFR-mutated non-small cell lung cancer. In patients with previously untreated egfr-mutated NSCLC, the combination of RYBREVANT® and Lazertinib demonstrated a statistically significant and clinically meaningful improvement in progression-free survival compared to ositinib.
Clinical Trials
AMAZE-lung (NCT05601973)
Trial Duration: from February 15, 2017 to May 10, 2019
PATIENT POPULATION: 181 patients aged 18 years and older. Enrolled patients received oral Lazertinib 20 mg (Part A), 320 mg (Part B), or 240 mg (Part C) consecutively once daily until disease progression, unacceptable toxicity, or other criteria for discontinuation were met.78 patients were treated with 240 mg of Lazertinib, and efficacy and safety could be assessed.
STUDY ENDPOINTS: The primary endpoints were safety and objective remission rate. Secondary endpoints included progression-free survival, overall survival, and intracranial objective remission rate.
FINDINGS: At data cutoff, the median duration of Lazertinib treatment was 13.3 months, and the mean relative dose intensity was 95.5%. Of the 78 patients, 19 continued treatment and 59 discontinued, most commonly due to disease progression.
Among T790M-positive patients (N = 76), the objective remission rate was 55.3%, complete remission was 1.3%, partial remission was 53.9%, stable disease was 34.2%, and disease progression was 7.9%; the median duration of remission was 17.7 months, with 27.6% of patients responding to Lazertinib for 12 months or longer; the disease control rate was 89.5%; and the compared to baseline Mean optimal percent change in tumor size compared to baseline -50.4%; median progression-free survival 11.1 months, with estimated PFS rates of 59.3%, 48.0%, and 38.0% at 6, 12, and 18 months, respectively. At a median follow-up time of 22.0 months, median overall survival had not been reached, with 12-month overall survival rates of 89.5% and 24-month overall survival rates of 72.7%. Among T790M-positive patients with measurable intracranial lesions assessed by an independent central review (n=7), the rate of objective intracranial remission was 85.7%, complete remission 14.3%, and partial remission 71.4%; the rate of intracranial disease control was 100%; the median duration of remission in response to the intracranial response was 15.1 months; and the median progression-free survival in the intracranial period was 26.0 months.
ADVERSE REACTIONS: In the Lazertinib treatment group at a dose of 240 mg/d, the most common adverse reactions of all grades included: rash (37.2%), pruritus (34.6%), abnormal sensation (33.3%), headache (28.2%), muscle cramps (28.2%), diarrhea (26.9%), decreased appetite (25.6%), onychomycosis ( 20.5%), cough (20.5%), constipation (19.2%), nausea (16.7%), fatigue (15.4%), elevated aspartate aminotransferase (14.1%), dizziness (12.8%), elevated alanine aminotransferase (12.8%), muscle aches (12.8%), dyspepsia (11.5%), stomatitis (11.5%), elevated blood creatinine (11.5%), dry skin (10.3%), vomiting (10.3%), and pulmonary embolism (10.3%).
Most common grade 3 adverse reactions: abnormal sensation (2.6%), rash (1.3%), cough (1.3%), diarrhea (1.3%), onychomycosis (1.3%), pulmonary embolism (1.3%). The most common Grade 4 or Grade 5 adverse reactions were both pulmonary embolism (1.3%).
LASER301 (NCT04248829).
Trial duration: February 13, 2020 - July 29, 2022 (substantially completed)
PATIENT POPULATION AND TRIAL METHODS: Patients ≥18 years of age with no prior systemic anticancer therapy. Patients with neurologically stable CNS metastases are allowed. Stratified by mutation status and ethnicity, patients were randomized in a 1:1 ratio to either lazertinib 240 mg daily oral or gefitinib 250 mg daily oral. The primary endpoint was progression-free survival (PFS) as assessed by the investigators of RECIST v1.1.
TRIAL RESULTS: 393 patients at 96 sites in 13 countries were treated in the double-blind study. Median PFS was significantly longer in the lazertinib group than in the gefitinib group (20.6 months vs. 9.7 months; hazard ratio [HR], 0.45; 95% CI, 0.34 ~ 0.58; P < 0.001). The PFS benefit of lazertinib versus gefitinib was consistent across all predefined subgroups. Objective efficacy was 76% in both groups (advantage ratio, 0.99; 95% CI, 0.62 ~ 1.59). The median duration of remission was 19.4 months (95% CI, 16.6 to 24.9) for lazertinib and 8.3 months (95% CI, 6.9 to 10.9) for gefitinib. Overall survival data were immature (29% mature) at the interim analysis. The 18-month survival rate was 80% in the lazertinib group and 72% in the gefitinib group (HR, 0.74; 95% CI, 0.51 to 1.08; P = 0.116). The observed safety of both treatments was consistent with previously reported safety.